Testosterone
What is testosterone?
Sources of testosterone
Make your own testosterone
MEN
WOMEN
Contraindications
References
What is testosterone?
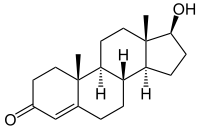
Testosterone is a steroid hormone made from a sterol called cholesterol. Most is produced in men's testes. Women also produce a little testosterone in their ovaries and adrenal glands - but only about 5-10% as much as men.
In both men and women, testosterone plays a crucial role in stimulating muscle growth; bone growth; energy production; the retention of electrolytes (sodium, potassium, and chloride) and nitrogen; and water retention in body fluid balance. Testosterone also affects the libido and mood, and when it declines they are negatively affected.
The small amount of testosterone naturally occurring in women does not have a masculinising effect.
Testosterone is an androgen, one of a group of hormones that control masculine sex characteristics. In men, these androgens promote muscle growth, the development of a deeper voice, testicles, and facial and body hair. Testosterone stimulates men's libido, sexual function, body shape, mood and energy levels. Testosterone makes the veins under the skin more prominent and the skin less fatty. It is essential for the development and maintenance of the male sex organs and the male secondary sex characteristics.
In both men and women, testosterone production occurs during the night and early morning, and is therefore at its highest level upon waking. The high level of testosterone in the morning explains why healthy men often wake with an erection. Blood serum testosterone level slowly decreases during the day and is at its lowest in the late afternoon or early evening.
After the glands produce testosterone, it is secreted into the blood. 99% of it is quickly adhered to by a protein sex hormone-binding globulin (SHBG), which acts as a carrier to move hormones around the body. The remaining 1% (free testosterone) is bio-available to act on and enter into cells throughout the body.
Testosterone level can be measured with a blood test, and it should preferably be taken in the morning when testosterone level is the highest. If possible it is best to measure both the SHBG bound testosterone and the free testosterone levels. If only the total testosterone is measured, you do not get an accurate representation of how much testosterone is free to act in the body. It is the levels of free testosterone and SHBG that determine how effective testosterone is in the body.
Sources of testosterone
Pure testosterone is not found in any plants. In other words, you cannot use any plant as a direct source of testosterone. However it is possible to reverse falling or low levels of testosterone by using plants high in androgens, androgen stimulants, steroidal precursors, and vitamins (particularly B5). Phytoandrogens are plants that contain androgens, or that stimulate androgenic activity. They increase the body's levels of free testosterone, and raise the androgen/estrogen balance.
Testosterone was first manufactured in the late 1930's. Today, soy bean substrates are used to manufacture natural testosterone. Natural/genuine/pure/bio-identical testosterone cannot be patented.
Note: Excess levels of testosterone are converted into estrogen by an enzyme called aromatase. This is a good reason not to overdose with testosterone, as it can cause the horrible symptoms of estrogen dominance.
Warning. The pharmaceutical industry has developed a number of testosterone look-alikes, so that they can patent them. These synthetic testosterone analogues (look-alikes) are not naturally-occurring and have a molecule that is different to that of real testosterone. This difference means that they can be patented, owned, and sold at a higher price. The altered molecules have testosterone-like activities, but unlike natural testosterone, these pharmaceutical testosterone analogues are not as effective as the real thing. More importantly they have a variety of nasty side-effects including low sperm count / sterility. They include fluoxymesterone and methyltestosterone. Some doctors are not aware of this crucial difference between natural bio-identical testosterone and the patented look-alikes. It is absolutely critical that you always use the real thing - natural or bio-identical hormones. (3)
Make your own testosterone
You can assist your body to make its own testosterone in several ways:
- Supporting your adrenal glands, and their production of DHEA which is used as a building material for testosterone. Adrenal exhaustion lowers your testosterone.
- Reducing your stress level, and the ongoing level of cortisol in your body. See adrenal exhaustion above, and other ways to de-stress such as meditation and relaxing postures. High levels of cortisol lower the production of testosterone.
- Getting plenty of sleep and rest. Rest literally builds testosterone.
- Reduce your exposure to xenoestrogens. This is the term for a wide range of estrogen-like polluting chemicals in our food, water and environment (plastics, pesticides, household chemicals etc) which are able to fool the estrogen receptors in cells, with disastrous results. They are anti-androgenic, blocking the action of testosterone. Various estrogenic foods are also discussed in the above link.
- Ensure you have sufficient protein in your diet. People on low protein diets tend to have higher levels of sex hormone binding globulin (SHBG), which binds to and inactivates testosterone. This is often a problem for older people, or those on strict vegetarian or vegan diets. A high level of fibre in the diet also increases the level of SHBG.
- Ensure you have sufficient saturated fat in your diet. Saturated fat and cholesterol are the building materials for steroidal hormones.
- Ensure you have sufficient carbohydrates in your diet. In one study (13), the researchers divided their subjects into 2 groups. One group ate a high-carb low-protein diet, the other group ate a high-protein low-carb diet. Fat intake and calories were identical in each group. After ten days the high-carb group had significantly higher free testosterone levels (+36%), lower SHBG levels and lower cortisol levels compared to the high-protein low-carb group.
Another study (14) showed that in exercising men, the stress hormone cortisol increased rapidly when they were put on a very low-carb diet. As cortisol increases, the level of testosterone decreases. - Being overweight or obese tends to increase estrogen dominance, which inhibits testosterone.
- Foods and herbs that assist androgen sufficiency include:
Pine is the plant that has the highest level of phytoandrogens discovered so far, with pine pollen being the richest and most convenient source. Pine kernels (seeds) are also a good source of phytoandrogens, and delicious to eat too. All species of pine are suitable, with the most popular species being Pinus sylvestris and P. nigra in the USA, P. massonia and P. tabulaeformis in China, and P. koraiensis in Korea.
Ashwagandha.
Ginseng (Panax ginseng).
Tienchi Ginseng (Panax notoginseng).
Siberian Ginseng (Eleutherococcus senticosus, Acanthopanax senticosus).
Nettle root (Urtica dioica).
Tribulus (Tribulus terrestris).
Celery. Juice 3-4 stalks per day to use it as a supplement. It also lowers blood pressure, improves kidney function, is an anti-inflammatory, a diuretic and a gout treatment.
Corn. The kernels, silk and pollen may all be used. Corn is a tonic for the whole urinary tract and the adrenal glands. It is a remedy for urinary tract infections, cystitis, bladder infections and prostatitis. It is a soothing anti-inflammatory and diuretic. Juice the raw corn kernels, eat the beard.
Cucumber. Do not peel, juice or eat whole. Cucumbers contain a high level of silica and act as a kidney tonic, and are great for your skin, keeping it elastic.
Spinach, radish, garlic and red meat are other foods that promote androgenic hormones and assist the androgen/estrogen ratio.
- Zinc sufficiency is important for male sexual health. The best foods from which to get zinc include oysters, seafood, lamb, pumpkin seeds and tree nuts.
- Sufficient vitamin D and sufficient magnesium are required to make your own testosterone.
- Reducing or avoiding alcohol. After a period of heavy drinking the liver may recover, but the testes less so.
MEN
Symptoms of low testosterone in men
Causes of / risk factors for low testosterone in men
Aging in men
Testosterone replacement therapy (TRT) for men
Side-effects from excessive testosterone in men
Should men supplement with progesterone rather than testosterone?
Symptoms of low testosterone in men
- Fatigue.
- Low energy and lethargy.
- Muscle strength diminished.
- Muscle bulk/mass decreased.
- Change of body shape, with increased abdominal fat and rudimentary breast development (man boobs).
- Body hair decreased (feminisation).
- Mood changes, ill temper, depression (15), loss of feeling of wellbeing and optimism. Poor memory performance. Decreased cognitive status, mental acuity and clear thinking.
- Erectile dysfunction - difficulty getting and maintaining an erection.
- Low libido, loss of sexual interest.
- Low sperm count in semen.
- Osteoporosis or decreased bone mineral density.
- Anaemia.
Causes of / risk factors for low testosterone in men

- Vitamin D deficiency.
- Ageing.
- Chronic stress.
- Insufficient sleep and rest.
- Lack of regular exercise and lack of regular sex. Both these activities help in stimulating the body's production of its own testosterone.
- Pharmaceutical drugs (including glucocorticoids, opiates, anabolic steroids).
- Alcohol.
- Smoking.
- Severe trauma, illness, burns or major surgery.
Testicular damage (primary hypogonadism)
- Klinefelter's syndrome (when males have an extra X chromosome).
- Cryptorchidism (the absence of one or both testes from the scrotum).
- Problems during testis development (twisted or strangulated testes).
- Orchitis (inflammation of the testes).
- Orchidectomy (testes surgically removed).
- Toxic damage (EMF radiation, chemotherapy, industrial or environmental toxins).
Brain disorders (secondary hypogonadism)
- Pituitary gland malfunction.
- Hypothalamus malfunction.
- Kallmann's syndrome (genetic disorder of sex glands).
- Haemochromatosis (Blood iron excess disorder).
- Brain tumour.
Aging in men
Healthy men continue to produce testosterone throughout their lives, but at a slowly decreasing rate. Young men have high levels of testosterone and old men have lower levels.
Testosterone does not cause prostate cancer or BPH. If testosterone were the cause, young men (who have much higher levels of testosterone than old men) would be suffering from enlarged prostates and prostate cancer. Studies show that older men with the highest level of testosterone have the least prostate enlargement. Conversely, men with the highest level of estrogen have enlarged prostates.
As most men age, the level of estrogens, estrogen look-alikes and xenoestrogen toxins in their bodies rises. Declining testosterone from aging, together with this increasing level of various estrogens, is the most likely cause of prostate enlargement and prostate cancer in men.
Over a third of all men over the age of forty show some symptoms of testosterone deficiency. They are middle aged and older men who have symptoms associated with low testosterone levels but do not have primary or secondary hypogonadism. Their symptoms are often non-specific, and can be further complicated by pre-existing medical conditions such as obesity, diabetes and other chronic illness. These men typically complain of lethargy and low energy, insomnia and sleep disturbance, low libido, irritability, anxiety, reduced concentration and an unhappy mood.
Here are reference ranges for the hormones oestradiol, testosterone and progesterone for men:
Oestradiol 0.5 - 2.2 pg/ml
Progesterone 15 - 100 pg/ml
Testosterone 44 - 148 pg/ml
Testosterone replacement therapy (TRT) for men
Testosterone replacement therapy may be appropriate in those cases where a patient's blood testosterone level is low, and additional tests show that symptoms of hypogonadism are present. It is essential that a diagnosis and a decision on whether to use testosterone is NOT made on the result of a blood test alone.
Many doctors assume that testosterone is not an issue if a patient's blood testosterone test is at a level towards the low end of the "normal" range. Older men in particular often remain undiagnosed because they often have a blood testosterone level that is low but not low enough to alert the medical practitioner to the real causes. So doctors often treat them by prescribing anti-depressants or other drugs, rather than correcting the estrogen build-up and the borderline low level of testosterone.
If you are experiencing any symptoms of low testosterone and have a low or borderline level of testosterone, then first ensure that you have a good level of vitamin D and other factors mentioned on this web page. If you decide to use a hormone supplement, I recommend first considering the use of progesterone rather than testosterone.
There is little evidence that testosterone is the most effective means of restoring energy, libido and sexual response in men with marginally low testosterone levels. Progesterone, rather than testosterone, is likely to be more effective. In both men and women there is a correlation between progesterone and testosterone levels. (11,12)
A study (9) showed that when testosterone therapy is used in older men to boost their energy and vitality, there is a significantly increased risk of cardiovascular, respiratory and dermatological problems. The research examined men 65 or older with impaired mobility and increased health risks, who had taken testosterone supplements. This contradicts other publications portraying testosterone as the elixir of youth and vitality, showing that testosterone therapy in older men is beneficial for the cardiovascular system, and improves sexual function, mood, energy level, and muscle and bone mass and strength. The study confirmed the general wisdom that a daily topical dosage of 50-150 mg of testosterone results in a level of serum testosterone (mean 574 ng/dL) that would be considered healthy in young men. However, when testosterone is applied topically as a cream the blood capillary level is 10-20 times higher than venous blood levels, and salivary testosterone levels are even higher! The bottom line: very little testosterone should be taken topically (through the skin), even though this is the best way to take it as a supplement.
Testosterone supplements have been used to treat men for many decades. The most patient-friendly and flexible form of treatment is testosterone skin cream. It can be applied directly to the skin of the scrotum or other receptive areas. Gels and creams have mostly replaced other forms of testosterone. For example, injections can be painful and do not provide a consistent level of testosterone in the following days and weeks; patches have a high level of adverse skin reactions and are unsightly; pellets need surgical application, can become infected, may be painful, and can fall out; oral capsules may be erratically absorbed, poorly tolerated in the gastrointestinal system, and do not provide consistent testosterone levels.
Side-effects from excessive testosterone in men
- Vomiting or nausea.
- Acne.
- Swelling of the ankles.
- Headaches.
- Excessive or increased appetite.
- Breast development, also known as gynecomastia.
- Persistent or too frequent erections (priapism).
- Reduction in sperm.
- Hair loss.
- Symptoms of mania - an abnormally elevated (or irritable) mood, arousal or energy level.
- Raised blood fat (serum lipid) level. This is NOT normally a risk of using natural testosterone, however, it is a risk when using pharmaceutical testosterone analogues or look-alikes.
- Decreased HDL cholesterol level.
- Increased estradiol levels.
- Increased level of dihydrotestosterone (DHT), a potent endogenous androgenic hormone derived from testosterone.
- Abnormal increase in red blood cells (polycythemia). Men with hypogonadism tend to have anaemia and testosterone replacement corrects the low red blood cell level. However, too high a dose of testosterone, even for a short period, can lead to polycythemia. The effect is not life-threatening, but should be monitored by your doctor.
- Increased prostate size, mainly during the first six months of treatment. This should not be a problem because men with low testosterone usually have a slightly smaller prostate that returns to normal size during treatment. There is no evidence to suggest that replacement of low testosterone levels back to the normal range leads to any increase in the occurrence of prostate cancer or high levels of prostate specific antigen (PSA). PSA is often below normal in hypogonadal men and is generally restored to normal levels with testosterone supplementation.
- Heart, lung and skin abnormalities. A study (4) showed that when topical testosterone therapy is used in older men there is a significantly increased risk of cardiovascular, respiratory and dermatological problems.
Should men supplement with progesterone rather than testosterone?
Any man considering supplementing with testosterone should first consider whether progesterone is a better alternative. In both men and women progesterone is the hormone that "drives" the level of testosterone, and correcting the level of progesterone, vitamin D and any other major deficiences is usually the key to healing the patient's symptoms.
Men's testosterone levels are at their highest point in their early 20's. From this peak, testosterone levels decline rapidly through to the late twenty's. Thereafter testosterone continues to decline, but at a slower rate.
As a man ages his testosterone is increasingly converted into di-hydrotestosterone (DHT) by 5-alpha-reductase. High levels of testosterone and DHT are both associated with benign prostatic hyperplasia (BPH) and cancer. Testosterone promotes prostate cell proliferation (9), although relatively low levels of serum testosterone are found in patients with BPH (5,6). The action of DHT is probably 10 times more potent in causing BPH.
Progesterone is a natural inhibitor of 5-alpha-reductase. Much better than pharmaceutical 5-alpha reductase inhibitors such as finasteride! (Pharmaceutical drugs almost always have nasty side-effects).
A man's estrogen levels also increase as he ages. Oestrogen stimulates the growth of hormonally-sensitive cells such as the prostate and breasts (man boobs). Hyperplasia or cancers are associated with high levels of estrogen or xenoestrogens (numerous estrogen look-alikes). There is no definitive research here, but it is probably estrogen dominance that is the main cause of BPH, along with the DHT.
Progesterone is a powerful estrogen-inhibitor.
For the above two reasons, progesterone is an excellent choice for men. It is not just a "female hormone" but is also essential to preserve masculinity! Progesterone for men becomes even more important with age. The aim of progesterone supplementation is to re-establish normal levels of both testosterone and progesterone. This will regain energy and strength, sexual function and libido, correction of anaemia, brain health (wellbeing and optimism, improvement in memory performance and cognitive status, mental acuity, clear thinking) and physical status (reduction in fat and increase in lean body mass muscle bulk and strength, male body characteristics, increase in bone mineral density) by the most effective and risk-free means available.
Another study (12) showed that it is progesterone, and not testosterone or oestradiol that facilitates penis erection.
WOMEN
 Symptoms of low testosterone in women
Symptoms of low testosterone in women
Causes of / risk factors for low testosterone in women
Before using testosterone treatment for women
Testosterone replacement therapy (TRT) for women
Side-effects from testosterone supplementation in women
Should women supplement with progesterone rather than testosterone?
Three main hormones (progesterone, estrogen and testosterone) operate in a woman's body. They play a vital role in a woman's sexual behaviour, enhancing her interest in initiating sexual activity and in her response to sexual stimulation. Sufficiency of these hormones are also associated with increased energy and vitality, a feeling of greater well-being and with reduced anxiety and depression.
The testosterone level in a woman peaks at about the age of 20. By the age of 40, it is about half the peak level, and it continues to fall as the years go by.
A woman's testosterone level rises gradually from about the 24th day of her menstrual cycle until ovulation on about the 14th day of the next cycle. In the week after ovulation her testosterone level is the lowest. Her libido increases with the progesterone over this period. (11) Low estrogen at this time may cause less natural lubrication.
Low libido, unexplained fatigue and lack of energy may be associated with low testosterone in peri-menopausal and post-menopausal women. However, supplementation with testosterone is not the most effective way to correct this situation. Research (11) shows that it is progesterone that 'drives' the level of the other hormones, and there is a correlation between the levels of progesterone and testosterone.
Here are reference ranges for oestradiol, testosterone and progesterone for women:
Pre-menopausal
Oestradiol 1.3 - 3.3 pg/ml
Progesterone 75 - 270 pg/ml
Testosterone 16 - 55 pg/ml
Post-menopausal
Oestradiol 0.5 - 1.7 pg/ml
Progesterone 12 - 100 pg/ml
Testosterone 16 - 55 pg/ml
Symptoms of low testosterone in women
- Low libido, loss of sexual desire, lack of arousal, anorgasmia (inability to have orgasms), vaginal dryness.
- Loss of muscle strength and mass.
- Accumulation of fat, especially around the abdomen.
- Osteoporosis, osteopenia and related bone deterioration.
- Insomnia.
- Fatigue, exhaustion.
- Diminished motivation and drive. Decreased sense of personal wellbeing. Depression, mood swings, anxiety. Hopelessness. Lack of concentration. (15)
Causes of / risk factors for low testosterone in women
- Aging.
- Hysterectomy. Removal of the ovaries causes an immediate 50% reduction in serum testosterone level.
- Insufficient sleep and rest.
- Premature ovarian failure (early menopause).
- Vitamin D deficiency.
- Oral contraceptives or any other medications containing estrogen.
- Various non-hormonal pharmaceutical medications. Eg: the anticonvulsant phenytoin.
- Thyroxine tablets (thyroid hormone).
- Diabetes.
- Severe or morbid obesity.
- Hypertension (high blood pressure).
- Stress.
- Lack of regular exercise and lack of regular sex. Both these activities help in stimulating the body's production of its own testosterone.
- Infections such as mumps, meningitis or syphilis.
- Alcohol.
- Smoking.
- Pregnancy.
- Reduced liver function.
- Severe trauma, illness, burns or major surgery.
- Ovarian cancer and subsequent chemotherapy / radiation treatment.
- Various malfunctions, malformation or diseases of the adrenal glands, pituitary gland in the brain, or some other glands.
Before using testosterone treatment for women

I don't recommend that women supplement with testosterone, because the adult female body can make its own testosterone from progesterone. This is safer, avoids testosterone overdose, and avoids the risk of side-effects from testosterone supplementation. However, your body can only use real progesterone. It is not able to use synthetic pharmaceutical progesterone look-alikes, such as progestin and progestogen. To repeat, if you use an altered progesterone lookalike it will NOT correct your testosterone level. Pharmaceutical companies deliberately name their products with confusingly similar names, and have successfully duped most doctors. For this reason, most doctors are unaware of how easy it is to correct a woman's testosterone levels with (real) progesterone.
If you decide to use testosterone supplementation regardless, it is important to first rule out other possible causes of your symptoms. Usually your symptoms will be caused by other factors. This requires an extensive examination by a trained medical practitioner. A pap smear, serum thyroid stimulating hormone TSH), and full blood examination including iron should be obtained. Issues to discuss include alternative treatments for sexual dysfunction, lack of vaginal lubrication or muscle tone, etc. Conditions such as iron deficiency, breast lumps, low bone density, depression, abnormal bleeding, diabetes, thyroid or adrenal disease need to be investigated before using testosterone.
It is extremely unlikely that a woman will be deficient in testosterone without an imbalance in her other hormones. According to one paper, "No single androgen level is predictive of low female sexual function." (10) Usually her symptoms will be caused by an imbalance in a variety of hormones. Supplementing with testosterone alone will probably NOT correct the symptoms, and testosterone is seldom the most appropriate hormone to supplement.
Testosterone replacement therapy (TRT) for women
After about 1970, it was standard medical practice to supplement with estrogen after removal of the ovaries, but ignore the hormones testosterone and progesterone. Estrogen supplementation does not usually restore libido in oophorectomised women. Eventually doctors started supplementing testosterone in the form of injections and implants. It was therapeutically effective, but because serum levels could not be closely controlled there were some serious side-effects such as masculinisation, hirsutism (body hair growth), acne and voice changes.
In Europe and Australia, a 1% testosterone cream is the preferred choice of most doctors and their female patients. Injections, implants and patches all have disadvantages compared to the cream. They can deliver an unstable dose, causing side effects; injections and implants can be painful; patches unsightly. Creams are invisible and painless, and the dose is both accurate and can be precisely tailored to the patient's specific needs.
Small amounts of testosterone have been used to manage low libido in women for decades. However, there is little evidence that it is the most effective means of restoring energy, libido and sexual response in women with low testosterone levels. Progesterone, rather than testosterone, is more effective at raising libido for both men and women.
Side-effects from testosterone supplementation in women
Women seldom need supplemental testosterone. The following side-effects are usually the result of sustained high-dose testosterone supplementation (especially injections) causing blood levels to exceed the normal upper limits for extended periods. But even low levels of testosterone supplementation raise the risk of the following symptoms:
- Nausea and vomiting.
- Headaches.
- Jaundice.
- Swelling of joints.
- Development of masculine characteristics such as increased muscle bulk, increased body and facial hair, and deepening of the voice.
- Hirsutism (increased body and facial hair).
- Loss of scalp hair (balding).
- Belly fat. The accumulation of visceral fat in middle-aged and post-menopausal women. (7)
- Adult acne.
- Oily skin.
- Sleep apnoea - sleep disorder, abnormal pauses in breathing, low breathing.
- Insulin resistance or metabolic syndrome.
- Cardiovascular disease.
- Weight gain.
- Cancer.
Should women supplement with progesterone rather than testosterone?
Any woman considering supplementing with testosterone should first consider whether progesterone is a better alternative. I would not advise that a woman should take testosterone supplements unless her doctor has specific medical reasons to do this. The numerous benefits of progesterone are described on Grow Youthful's progesterone web page.
The use of testosterone supplements by women raises the risk of the negative side-effects listed above.
Contraindications
Patients with severe heart disease, liver disease or kidney disease should not use any kind of testosterone replacement therapy except under close medical supervision.
References
1. Goldstat R. et al.
Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women.
Menopause 2003; 10 (5): 390-398.
2. El-Hage et al.
A double-blind, randomised, placebo-controlled trial of the effect of testosterone cream on the sexual motivation of menopausal
hysterectomized women with hypoactive sexual desire disorder.
Climacteric 2007; 10: 335-343.
3. Kent Holtorf.
Bio-identical vs synthetic hormones.
Postgraduate Medicine, Volume 121, issue 1, January 2009, issn - 0032-5481, e-issn - 1941-9260 9.
4. Basaria S et.al.
Adverse Events Associated with Testosterone Administration.
N Eng J Med June 30, 2010.
5. Lagiou, Pagona; Mantzoros, Christos S.; Tzonou, Anastasia; Signorello, Lisa B.; Lipworth, Loren; Trichopoubs, Dimitrios.
Serum Steroids in Relation to Benign Prostatic Hyperplasia.
1997, Oncology 54 (6): 497-501. doi:10.1159/000227609. PMID 9394847.
6. Roberts, Rosebud O.; Jacobson, Debra J.; Rhodes, Thomas; Klee, George G.; Leiber, Michael M.; Jacobsen, Steven J.
Serum sex hormones and measures of benign prostatic hyperplasia.
2004, The Prostate 61 (2): 124-31. doi:10.1002/pros.20080. PMID 15305335.
7. Imke Janssen, Lynda H. Powell, Rasa Kazlauskaite, Sheila A. Dugan.
Testosterone and Visceral Fat in Midlife Women: The Study of Women's Health Across the Nation (SWAN) Fat Patterning Study.
Obesity (Silver Spring). 2010 March; 18(3): 604-610. Published online 2009 August 20. doi: 10.1038/oby.2009.251.
8. Shrita M. Patel, Sarah J. Ratcliffe, Muredach P. Reilly, Rachel Weinstein, Shalender Bhasin, Marc Blackman, Jane A. Cauley, Kim Sutton-Tyrrell, John Robbins, Linda P. Fried and Anne R. Cappola.
Higher Serum Testosterone Concentration in Older Women is Associated with Insulin Resistance, Metabolic Syndrome, and Cardiovascular Disease.
The Journal of Clinical Endocrinology & Metabolism. 1 December 2009, vol. 94 no. 12 4776-4784.
9. Feldman, Brian J.; Feldman, David.
The development of androgen-independent prostate cancer.
2001, Nature Reviews Cancer 1 (1): 34-45. doi:10.1038/35094009. PMID 11900250.
10. Davis SR, Davison SL, Donath S, Bell RJ.
Circulating androgen levels and self-reported sexual function in women.
JAMA. 2005 Jul 6;294(1):91-6.
11. Jeffrey D. Blaustein.
Progesterone and Progestin Receptors in the Brain: The Neglected Ones.
Endocrinology June 1, 2008 vol. 149 no. 6 2737-2738.
12. Andersen ML, Bignotto M, Tufik S.
Hormone treatment facilitates penile erection in castrated rats after sleep deprivation and cocaine.
J Neuroendocrinol. 2004 Feb;16(2):154-9.
13. Anderson KE, Rosner W, Khan MS, New MI, Pang SY, Wissel PS, Kappas A.
Diet-hormone interactions: protein/carbohydrate ratio alters reciprocally the plasma levels of testosterone and cortisol and their respective binding globulins in man.
Life Sci. 1987 May 4;40(18):1761-8.
14. Michael Gleeson, Nicolette C Bishop.
Special Feature for the Olympics: Effects of Excercise on the Immune System.
Immunology and Cell Biology (2000) 78, 554-561; doi:10.1111/j.1440-1711.2000.t01-6-x.
15. Andreas Walther, Jonas Breidenstein, Robert Miller.
Association of Testosterone Treatment With Alleviation of Depressive Symptoms in Men
A Systematic Review and Meta-analysis.
JAMA Psychiatry. Published online 14 November 2018. doi:10.1001/jamapsychiatry.2018.2734
