Atherosclerosis
What is atherosclerosis?
Atherosclerosis commonly affects these body parts
General symptoms of atherosclerosis
Risk factors for atherosclerosis
Causes of atherosclerosis
Evidence against the diet-heart hypothesis
Prevention / remedies / treatment for atherosclerosis
References
What is atherosclerosis?
Atherosclerosis is a disease of the arterial wall that narrows the artery. Raised patches or lesions called atherosclerotic plaques develop on the inner lining (endothelium) of the arterial wall. The plaques form like ulcers, and are made up of proteins (collagen, fibrin), dense cholesterol, oxidised fats, calcium phosphate and bacterial biofilm. They tend not to heal, alongside chronic, ongoing inflammation. In the worst cases these atherosclerotic plaques can completely constrict the artery, or can break away and block it.
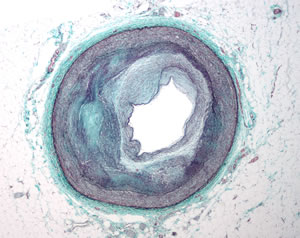
Atherosclerosis impairs blood flow through the arteries. The reduced blood flow can affect those parts of the body that depend on the affected arteries.
A century ago atherosclerosis used to be a problem affecting only the elderly, but today it can be found in some children entering their teens, and in the majority of middle-aged men and women.
Atherosclerosis commonly affects these body parts
The cardiovascular system. Atherosclerosis in the (coronary) arteries feeding the heart can cause angina, arrhythmia and heart attack (myocardial infarction). This is commonly referred to as coronary heart disease.
The brain. Constriction of the arteries feeding the brain can cause a stroke. Other symptoms include poor memory, neurological and cognitive problems.
The pelvis, arms and legs. Blockage of these peripheral arteries can cause cold hands and feet, numbness, painful muscles, ulcers and gangrene.
The intestines. Blockage of the arteries around the digestive tract can cause a variety of diseases, such as irritable bowel, abdominal pains, and even gangrene in the intestines.
The kidneys. Atherosclerosis in the arteries feeding the kidneys can cause high blood pressure, and kidney disease or failure. Changes in how you urinate (more often or less often), loss of appetite, nausea, swelling in the hands or feet, itching.
General symptoms of atherosclerosis
It is possible to suffer from atherosclerosis for years without showing any symptoms.
- Shortness of breath, difficulty breathing, being unfit.
- Fatigue (tiredness), lack of energy, trouble concentrating.
- Sleep problems, insomnia.
- Blood vessels visible under the skin.
- Smooth, shiny skin, and dry skin.
- Infections leading to gangrene in areas below the blocked artery.
- Thick nails, especially toe nails.
- Yellowish ring around the iris in the eye, also in the white of the eye.
- Hair loss.
- Erectile dysfunction.
Risk factors for atherosclerosis
- Diabetes or metabolic syndrome.
- Obesity.
- Hypertension (high blood pressure).
- Physical inactivity.
- Men are more prone than women.
- Family history.
- Chronic stress, or an anxious and aggressive personality.
- Smoking.
Causes of atherosclerosis
Conventional doctors and their medical associations maintain that the cause of atherosclerosis is not clear. Most of the research in the area is sponsored by the pharmaceutical and processed food industries, which stand to lose a lot of money if the current (flawed) explanation is exposed for what it is.
The current conventional and fatally-flawed advice is to avoid fats, especially saturated fats, and especially cholesterol. There is a mass of high quality scientific research which is NOT sponsored by the fast food and pharmaceutical industries, that shows that this low-saturated fat low-cholesterol diet is exactly the opposite of what is needed to prevent and heal atherosclerosis. (12, 14)
- Vitamin D and vitamin K2 deficiency. Vitamin K2 assists the body in putting calcium in bones and preventing it accumulating elsewhere, such as arterial plaque. Vitamins D and K2 assist in preventing osteoporosis. Vitamin K2 is produced by bacteria in a healthy gut biome, and the best food sources are:
high quality artisan hard cheeses made from raw milk, which contain a live bacterial culture and are not pasteurised,
butter from grass-fed cows,
meat from grass-fed animals,
raw sauerkraut. - A variety of spirochaete type bacteria and co-infected biofilms.
- Gum diseases, dental plaque / tartar / calculus. Poor dental hygiene, often initiated by vitamin C deficiency. (16, 17, 18, 19, 20)
- Toxins. Accumulation of a variety of toxins in the body. Foods are the most common and major source of toxins, usually accompanied by a variety of digestive problems. The main food source of toxins that produces atherosclerosis is plant lectins. Lectins are most concentrated in the skins and seeds of nightshades (like tomatoes, peppers and eggplants). However, there are also high levels in legumes, pulses, seeds and grains.
A range of estrogen-like hormones and chemicals (xenoestrogens) in the environment cause a numerous hormonal problems.
Many other toxic pollutants are found in our homes, everyday environment, personal care products and water. - Calcium deposits, nanobacteria.
- Omega-3 deficiency alongside excess Omega-6 polyunsaturated oils.
- Vitamin E deficiency.
- Copper deficiency and zinc to copper imbalance.
- Inflammation is also a symptom of the assault by the above causes. (12, 17, 21, 22)
Evidence against the diet-heart hypothesis
The retired professor of medicine and biochemistry at Vanderbilt University has described the diet-heart hypothesis as "the greatest scientific deception of our times". Discussing scientists whose deliberately deceptive research promotes the diet-heart hypothesis, he says "Fearing to lose their soft money funding, the academicians who should speak up and stop this wasteful anti-science are strangely quiet. Their silence has delayed a solution for coronary heart disease by a generation. (1, 2)
In 1991 a review (3) of more than 3000 references supporting the diet-heart campaign concluded that it was "based on fabrications, erroneous interpretations, and very importantly, the ignoring of massive amounts of unsupportive data." Further, "It does not seem possible that objective scientists without vested interests could ever interpret the literature as supportive... It is depressing to know that billions of dollars and a highly sophisticated medical research system are being wasted chasing windmills."
Another extensive review of all the available scientific literature was conducted and published as a book in 2000. (4) The conclusion? "Masses of valid scientific evidence should have destroyed the diet-heart idea by now... scientists who support the diet-heart idea and who are honest must be ignorant..."
Dr Natasha Campbell-McBride (5) has written a convincing book explaining why the diet-heart campaign is so enduring, and referencing hundreds of scientific papers showing that cholesterol is not a villain but is essential for our good health; that statins and other cholesterol-lowering drugs are extremely harmful; and that low-fat diets and the avoidance of saturated fats are the opposite of what we need for good health. (12, 13, 14)
Campbell-McBride refers to many studies that show that consuming animal fats protects against atherosclerosis and heart disease (and many other diseases). These studies show that eating vegetable oils (canola, corn, soy, cottonseed, peanut, rapeseed, sunflower) and margarine is strongly associated with heart disease (10, 11) - exactly the opposite of what the diet-heart campaign promotes. Many studies show that old people with high levels of cholesterol live longer than those with low cholesterol. (4) Reducing their cholesterol shortens their lives and causes a variety of diseases.
Prevention / remedies / treatment for atherosclerosis
- Diet. A non-toxic diet avoiding sugar and refined carbohydrates so you eat foods that starve rather than feed small-bacteria infections. Avoid using omega-6 polyunsaturated fats which cause systemic inflammation.
- Vitamin D.
- Probiotics. Get the best possible bacterial exposure, which also helps produce vitamin K2. Use probiotic foods and drinks throughout your life. Live, unpasteurised sauerkraut is recommended.
- Correct any omega-3 deficiency with an improved diet of grass fed meat, free-roaming natural habitat animal products, and the best food source of omega-3 fatty acids, wild-caught cold water oily fish. Avoid omega-6 polyunsaturated oils.
- Garlic
- Turmeric.
- Apple cider vinegar. (15)
- Vitamin B3 (niacin). Fish, beef, chicken, turkey and spirulina are the best food sources of niacin. In a more urgent situation, niacin can be purchased as a supplement, and may be useful at 500 mg per day in an extended-release form. Niacin is a powerful antioxidant which acts upon cholesterol, and in particular niacin decreases small, dense, oxidised forms of cholesterol. It provides cardiovascular protection by preventing white blood cells forming atherosclerotic accumulation. Niacin decreases triglyceride levels. It decreases vascular oxidation through its anti-inflammatory effects. Niacin decreases C-reactive protein, which is a strong predictor of heart attack, stroke and peripheral vascular disease. (21, 22, 23, 24, 25)
- Treatment of the causes of the inflammation, unique to you.
- Berberine.
- Vitamin C and other antioxidants. High doses of natural vitamin C are effective in clearing up atherosclerotic plaques, because they often tend to form when there is a deficiency of antioxidants, as in the modern diet.
- Copper sufficiency.
- Cholesterol. Getting sufficient cholesterol is essential.
- Citrus (lemon) bioflavonoids.
- Gum turpentine. An antimicrobial which can also remove biofilms.
- Earthing or grounding.
- See details of remedies recommended by Grow Youthful visitors, and their experience with them.
References
1. Mann George V.
Coronary Heart Disease: Doing the wrong things.
Nutrition today, July/August 1985, 12-14.
2. Mann George V., Shaffer R. D., Rich A.
Physical fitness and immunity to heart disease in Masai.
The Lancet 2, 1308-1310, 1965.
3. Smith Russell L.
Diet, blood cholesterol and coronary heart disease: a critical review of the literature.
Vector Enterprises, Vol 1 1989, vol 2 1991.
4. Ravnskov Uffe.
The Cholesterol Myths. Exposing the Fallacy that Saturated Fat and Cholesterol Cause Heart Disease.
New Trends Publishing, 2000.
5. Natasha Campbell-McBride.
Put Your Heart in Your Mouth.
Medinform Publishing, 2007.
6. Iribarren C. et al.
Serum total cholesterol and risk of hospitalisation and death from respiratory disease.
International Journal of Epidemiology 26, 1191-1202, 1997.
7. Iribarren C. et al.
Cohort study of serum total cholesterol and in-hospital incidence of infectious diseases.
Epidemiology and Infection 121, 335-347, 1998.
8. Elias E. R. et al.
Clinical effects of cholesterol supplementation in six patients with the Smith-Lemli-Opitz syndrome (SLOS).
American Journal of Medical Genetics 68, 305-310, 1997.
9. Horrobin David F.
Lowering cholesterol concentrations and mortality.
British Medical Journal 301, 554, 1990.
10. Pinckney ER.
The potential toxicity of excessive polyunsaturates. Do not let the patient harm himself.
American Heart Journal 85, 723-726, 1973.
11. West CE, Redgrave TG.
Reservations on the use of polyunsaturated fats in human nutrition.
Search 5, 90-96, 1974.
12. Aseem Malhotra, Rita F Redberg, Pascal Meier.
Saturated fat does not clog the arteries: coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventions.
Br J Sports Med Published Online First: 25 April 2017. doi: 10.1136/bjsports-2016-097285.
13. Rafel Ramos, Marc Comas-Cufi, Ruth Marti-Lluch, Elisabeth Ballo, Anna Ponjoan, Lia Alves-Cabratosa, Jordi Blanch, Jaume Marrugat, Roberto Elosua, Maria Grau, Marc Elosua-Bayes, Luis Garcia-Ortiz, Maria Garcia-Gil.
Statins for primary prevention of cardiovascular events and mortality in old and very old adults with and without type 2 diabetes: retrospective cohort study.
BMJ 2018;362:k3359. Published 5 September 2018.
14. Marinka Steur, Laura Johnson, Stephen J. Sharp, Fumiaki Imamura, Ivonne Sluijs, Timothy J. Key, Angela Wood, Rajiv Chowdhury, Marcela Guevara, Marianne U. Jakobsen et al.
Dietary Fatty Acids, Macronutrient Substitutions, Food Sources and Incidence of Coronary Heart Disease: Findings From the EPIC-CVD Case-Cohort Study Across Nine European Countries.
19 November 2021. Journal of the American Heart Association. 2021;0:e019814.
15. Setorki M, Asgary S, Eidi A, Rohani AH, Khazaei M.
Acute effects of vinegar intake on some biochemical risk factors of atherosclerosis in hypercholesterolemic rabbits.
Lipids Health Dis. 2010 Jan 28;9:10. doi: 10.1186/1476-511X-9-10. PMID: 20109192; PMCID: PMC2837006.
16. Chhibber-Goel J, Singhal V, Bhowmik D, Vivek R, Parakh N, Bhargava B, Sharma A.
Linkages between oral commensal bacteria and atherosclerotic plaques in coronary artery disease patients.
NPJ Biofilms Microbiomes. 2016 Dec 19;2:7. doi: 10.1038/s41522-016-0009-7. PMID: 28649401; PMCID: PMC5460270.
17. Zhou X, Li J, Guo J, et al.
Gut-dependent microbial translocation induces inflammation and cardiovascular events after ST-elevation myocardial infarction. Microbiome 6, 66 (2018). doi.org/10.1186/s40168-018-0441-4.
18. Tang WH, Kitai T, Hazen SL.
Gut Microbiota in Cardiovascular Health and Disease.
Circ Res. 31 March 2017; 120(7):1183-1196. doi: 10.1161/CIRCRESAHA.117.309715. PMID: 28360349; PMCID: PMC5390330.
19. Yang T, Santisteban MM, Rodriguez V, Li E, Ahmari N, Carvajal JM, Zadeh M, Gong M, Qi Y, Zubcevic J, Sahay B, Pepine CJ, Raizada MK, Mohamadzadeh M.
Gut dysbiosis is linked to hypertension.
Hypertension. 2015 Jun;65(6):1331-40. doi: 10.1161/HYPERTENSIONAHA.115.05315. Epub 13 April 2015. PMID: 25870193; PMCID: PMC4433416.
20. Wang G, Hao M, Liu Q, Jiang Y, Huang H, Yang G, Wang C.
Protective effect of recombinant Lactobacillus plantarum against H2O2-induced oxidative stress in HUVEC cells.
J Zhejiang Univ Sci B. 2021 May 15;22(5):348-365. doi: 10.1631/jzus.B2000441. PMID: 33973418; PMCID: PMC8110467.
21. Karacaglar E, Atar I, Altin C, Yetis B, Cakmak A, Bayraktar N, Coner A, Ozin B, Muderrisoglu H.
The Effects of Niacin on Inflammation in Patients with Non-ST Elevated Acute Coronary Syndrome.
Acta Cardiol Sin. 2015 Mar; 31(2):120-6. doi: 10.6515/acs20140630e. PMID: 27122858; PMCID: PMC4804877.
22. Si Y, Zhang Y, Zhao J, Guo S, Zhai L, Yao S, Sang H, Yang N, Song G, Gu J, Qin S.
Niacin inhibits vascular inflammation via downregulating nuclear transcription factor-kB signaling pathway.
Mediators Inflamm. 2014;2014:263786. doi: 10.1155/2014/263786. 27 May 2014. PMID: 24991087; PMCID: PMC4058495.
23. Canner PL, Berge KG, Wenger NK, Stamler J, Friedman L, Prineas RJ, Friedewald W.
Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin.
J Am Coll Cardiol. 1986 Dec;8(6):1245-55. doi: 10.1016/s0735-1097(86)80293-5. PMID: 3782631.
24. Berge KG, Canner PL.
Coronary drug project: experience with niacin. Coronary Drug Project Research Group.
Eur J Clin Pharmacol. 1991;40 Suppl 1:S49-51. PMID: 2044644.
25. Ganji SH, Qin S, Zhang L, Kamanna VS, Kashyap ML.
Niacin inhibits vascular oxidative stress, redox-sensitive genes, and monocyte adhesion to human aortic endothelial cells.
Atherosclerosis. 2009 Jan;202(1):68-75. doi: 10.1016/j.atherosclerosis.2008.04.044. Epub 2008 May 9. PMID: 18550065.
